Get support for
access and savings
Get details on financial assistance,
coverage, specialty pharmacies,
and more.
For men and postmenopausal women
with osteoporosis at high risk for fracture
For men and postmenopausal women
with osteoporosis at high risk for fracture
Savings Card
Add to the bone for as little as $0 a month*†
Eligible commercially insured patients may pay as little as $0 a month for their TYMLOS prescription.*† Simply fill out the form below to get your card. Be sure to read the patient instructions on the back of the card to redeem the offer.
This program is available only for prescriptions covered by commercial or private health insurance. If your insurance doesn’t cover TYMLOS:
- Call your insurance company to let them know you are interested in TYMLOS
- Contact Radius Assist to see if there are other ways to save on your medication
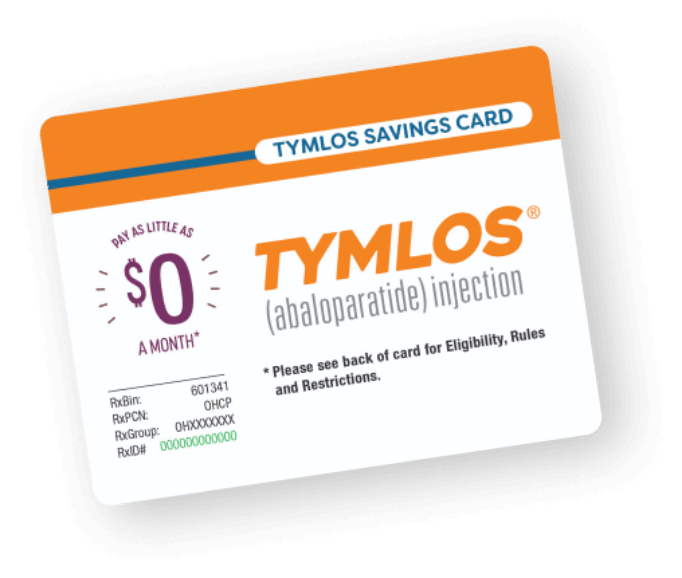
*There is an annual cap on the amount of assistance the patients can receive over a 1-year period.
View terms and conditions below
†This offer is not valid for patients using Medicare, Medicaid, or other government programs. See back of savings card for all eligibility requirements, rules, and restrictions.
Coverage and Access Information
Will my insurance cover TYMLOS?
TYMLOS is covered by 90% of commercial insurance plans and most Medicare Part D patients have access to TYMLOS.‡
Individual plan requirements and out-of-pocket costs will vary.
 (opens in a new tab)
(opens in a new tab)- Radius Assist is an assistance program that may help those who cannot afford their medication
- It provides TYMLOS (abaloparatide) injection therapy at no cost to qualified patients in need
- To qualify, patients must meet the eligibility criteria and, along with their healthcare provider, submit all required documentation
- If a patient is accepted into the program, they will receive at least 3 months of medication per shipment, and up to 24 months of therapy. Acceptance into the program is valid for the current calendar year and with a valid prescription (subject to continued eligibility) and until the patient has reached a total of 24 months of therapy provided by Radius Assist§
- Call Radius Assist at 1-866-896-5674
Questions about TYMLOS?
For reporting possible side effects, product complaints, or requesting additional Radius product information, please contact Radius Medical Support at 1-855-672-3487.
‡Data courtesy of Managed Markets Insight & Technology as of June 2025.
§Eligibility criteria for the Radius Assist Patient Assistance Program is subject to change at any time. Criteria changes will impact new patients entering the program and those that need to submit re-verifications for the next calendar year. Patients can receive up to, but not exceeding, 24 months of total TYMLOS therapy from Radius Assist. Radius Assist will discontinue providing therapy once the patient’s cumulative lifetime use of TYMLOS has reached 24 months. Use of TYMLOS for more than 2 years during a patient’s lifetime is not recommended.
What is a Specialty Pharmacy?
TYMLOS is a specialty medication that is prescribed through a Specialty Pharmacy, which is different from your local pharmacy. It dispenses medications that need more support than those dispensed from your local pharmacy. Your Specialty Pharmacy will walk you through the fulfillment process and schedule delivery of TYMLOS.
Once your doctor prescribes TYMLOS, you should expect a call from your Specialty Pharmacy
- A care coordinator will call you once they receive the prescription to verify your information
- The call may come from an unfamiliar number, like an 800 number or “unknown”
- After the call, save the Specialty Pharmacy number in your phone or write it down somewhere for future reference
- Your Specialty Pharmacy will work with you throughout your TYMLOS journey on any questions you have about your prescription and refills
Your Specialty Pharmacy will work with you throughout your TYMLOS journey on any questions you have about your prescription and refills.
If your medication requires prior authorization (most specialty medications do), your Specialty Pharmacy will work with your HCP and insurance provider to get approval and update you on the status.

Ready to talk about TYMLOS with your doctor?
If you’re at a high risk for fracture due to osteoporosis,
we can help start the conversation

Experience 1-on-1 injection support from our Clinical Educators
Prescribed TYMLOS? Sign up now for personalized support
and training from our TYMLOS Clinical Educators!
Connect with us: (opens in a new tab)
(opens in a new tab)
Terms and Conditions
TYMLOS® (abaloparatide) Patient Savings Card Program Terms and Conditions
With this TYMLOS Patient Savings Card, eligible commercially insured patients may pay as little as $0 per month in out-of-pocket costs for their TYMLOS prescription. There is an annual cap on the amount of assistance that patients can receive over a per calendar year period.
Patient Instructions: In order to redeem this offer, you must have a valid prescription for TYMLOS. Follow the dosage instructions given by the doctor. By using this offer, you agree that you meet the eligibility criteria and will comply with the Eligibility, Rules, and Restrictions section below each time you use this offer. Patients with questions about the TYMLOS Patient Savings Card offer should call 1-855-243-6222.
Pharmacist: When you apply this offer, you are certifying that you have not submitted a claim for reimbursement under any federal, state, or other governmental programs for this prescription. Participation in this program must comply with all applicable laws and regulations as a pharmacy provider. By participating in this program, you are certifying that you will comply with the terms and conditions described in the Eligibility, Rules, and Restrictions section below.
Pharmacist instructions for a patient with an Eligible Third-Party Payer: This card must be accompanied by a valid prescription for TYMLOS. Submit the claim to the primary Third-Party Payer first, then submit the balance as a secondary transaction to BIN 601341. The patient will be responsible for any remaining amount above the per calendar year cap. Valid Other Coverage Code required. Pharmacists with questions, please call 1-800-364-4767.
Eligibility, Rules, and Restrictions: Patients must be 18 years or older, and have a valid prescription for TYMLOS. There is an annual cap on the amount of assistance that patients can receive over a calendar-year period. This program is available only for prescriptions covered by commercial or private health insurance. This program is not available for prescriptions covered by state or federal government- funded healthcare programs, such as Medicare (including Part D), Medicare Advantage, Medigap, Medicaid, TRICARE, Department of Defense, and Veterans Administration. The patient understands that if they begin to receive drug benefits under any such government-funded program, they can no longer use this offer. The patient also agrees to follow any health insurance plan requirements, including telling their plan how much co-pay support they get from this program.
By redeeming this offer, the patient agrees that this program is intended solely for the benefit of the patient. Some insurance plans have established programs referred to as “accumulator adjustment” or “co-pay maximizer” programs that attempt to dilute the impact of the assistance available under this program. An accumulator adjustment program is one in which payments made by the patient that are subsidized by manufacturer assistance do not count toward the patient’s deductibles and other out-of-pocket cost sharing limitations. Co-pay maximizers are programs in which the amount of the patient’s out-of-pocket costs is increased to reflect the availability of support offered by a manufacturer assistance program. In those situations, the TYMLOS Patient Savings Card program terms may change at any time without notice in order to ensure the program remains focused on helping patients.
This offer is not transferable and is limited to one offer per person. Patients may not seek payment for the value of this offer from a third-party, such as a flexible spending account. This offer is only valid in the United States and is not valid in any state where it is prohibited by law. This card is not health insurance. The program may change or end at any time without notice. This offer may not be used with any other coupon, discount, prescription savings card, free trial, or other offer.
