Resources and support
for patients prescribed TYMLOS.
TYMLOS patient support—there
when you and your patients need it.
For men and postmenopausal women with osteoporosis at high risk for fracture

Not actual patients.
For men and postmenopausal women with osteoporosis at high risk for fracture
Jump to section
Prescribing resources and downloads.
How to Start Your Patients on TYMLOS
This guide outlines the steps on how to prescribe TYMLOS for your patients.
AACE Guidelines for Osteoanabolics
View AACE recommendations for when to consider abaloparatide for postmenopausal women with osteoporosis.
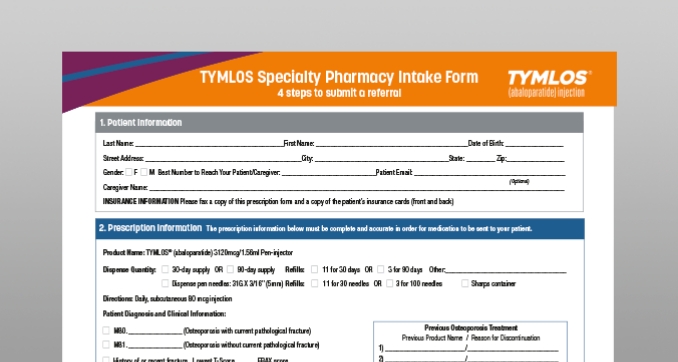
TYMLOS Specialty Pharmacy Intake Form
Complete this form and fax it directly to a specialty pharmacy that dispenses TYMLOS.
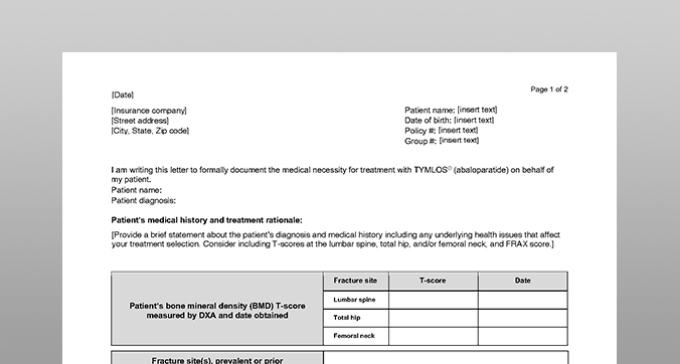
Sample of Prior Authorization (PA) Cover Letter
Some health plans require a PA request form in order to satisfy their policy requirements to obtain TYMLOS coverage. Use this sample letter as a template to help you get started.
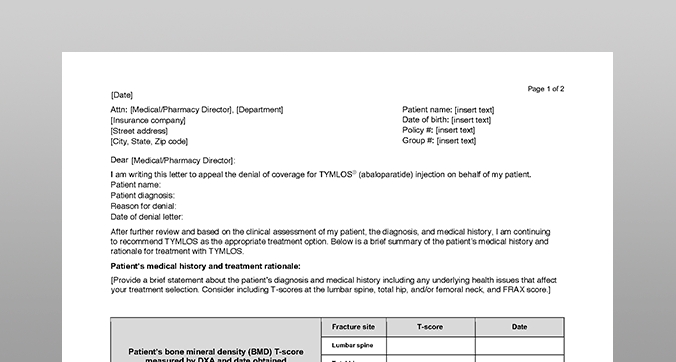
Sample Letter of Appeal
If a health plan denies TYMLOS coverage, they may require a letter of appeal along with a letter of medical necessity in order to reconsider the decision. This template can help you write your own letter of appeal.
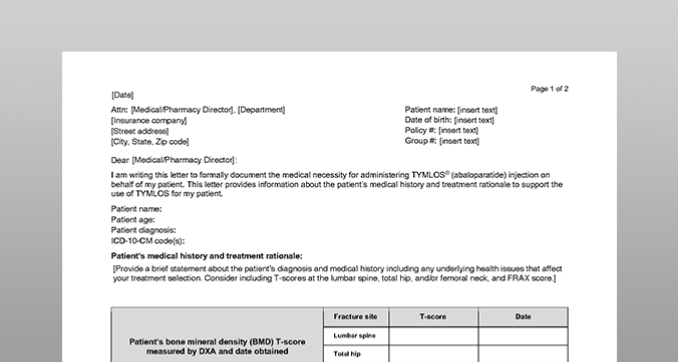
Sample Letter of Medical Necessity
Some health plans require a letter of medical necessity in addition to a letter of appeal that may help justify the clinical rationale for covering TYMLOS. Use this template to write a letter of medical necessity.

Brochure for Healthcare Professionals
Review the safety and efficacy for TYMLOS, as well as guidelines to help identify appropriate patients, and information about patient support in this brochure.
Download (opens in a new tab)Access and affordability.

Savings Card
Eligible,* commercially insured patients can pay as little as $0 a month for their TYMLOS prescription. There is an annual cap on the amount of assistance patients can receive over a 1-year period.1
*This offer is not valid for patients using Medicare, Medicaid, or other government-funded programs to pay for their medications. See back of Savings Card for all eligibility requirements, rules, and restrictions. Savings Card is available for patients to download at TYMLOS.com. Limited to one offer per person.1
TYMLOS Specialty Pharmacy (SP) Network List
See a list of non-integrated delivery network SPs that are able to dispense TYMLOS. In addition, SPs affiliated with an integrated delivery network are able to dispense TYMLOS.
TYMLOS is covered by most commercial and Medicare plans. Individual out-of-pocket costs will vary.1
Data courtesy of Managed Markets Insight & Technology as of January 3, 2024.
What to do if TYMLOS is not covered under your patient’s insurance plan?
Advise them to call 1‑866‑896‑5674
Visit the Radius Assist site (opens in a new tab) to learn more.
Do you have questions regarding Radius products?
Contact Radius Medical Support line: 1‑855‑672‑3487
Patient resources and downloads.

Encourage your patients to register for virtual injection training.
Injection training is provided through our Clinical Educator Network, which helps patients with a prescription understand how to use the pen and self-inject, and supports them as they start and stay on TYMLOS, as directed by you.
The TYMLOS Clinical Educators are also available to provide training for you and your staff on using the TYMLOS pen.
Connect to a Clinical Educator
Monday through Friday, 8 AM to 7 PM ET at
1‑855‑730‑8591
Encourage your patients to register for virtual training at www.TYMLOSsignup.com (opens in a new tab)
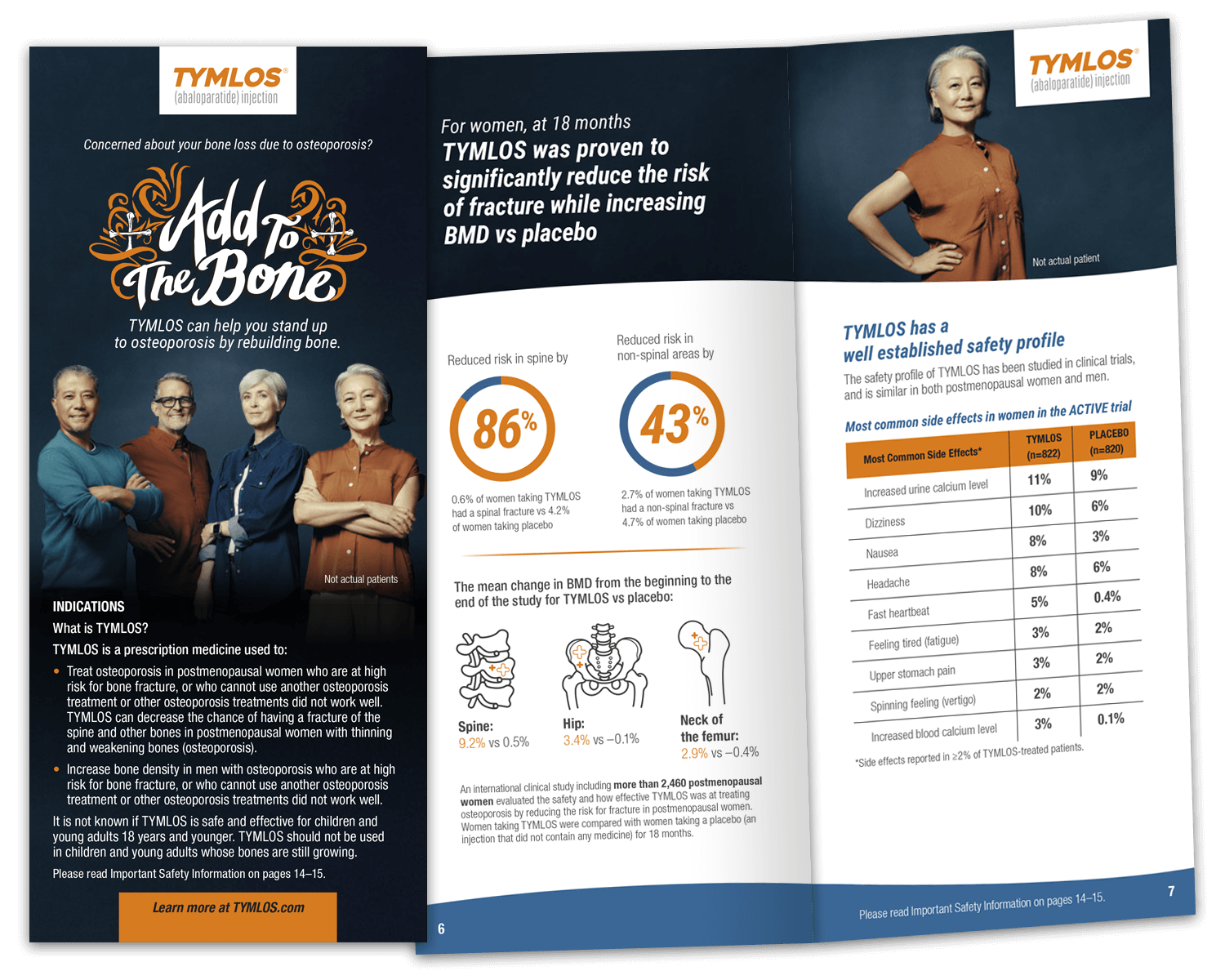
Patient Brochure
This brochure will help your patients understand osteoporosis as a disease, its associated risk factors, and the role TYMLOS plays in treating it. Inside, patients can find information on the TYMLOS patient support program, and directions on storage and use.
Need support or samples?
Let us know if you want to request samples or a visit from a TYMLOS representative or field reimbursement manager.